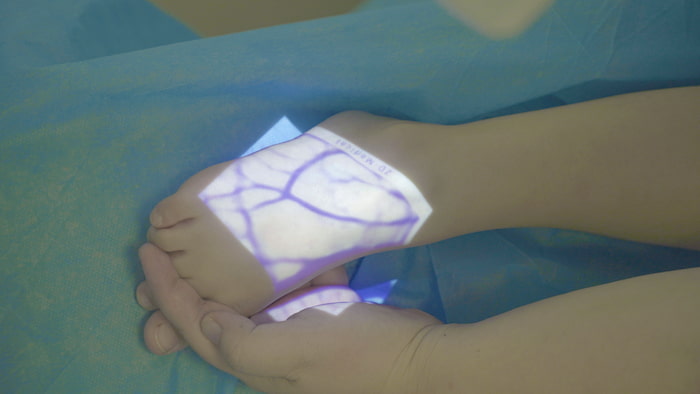
How can imaging technology be used to avoid scars and find available veins?
1-Near-Infrared Vein Finders
This is the most intuitive tool for dealing with superficial veins (within 10mm subcutaneous), such as Vein Finder
Working principle: Hemoglobin in the blood absorbs near-infrared light, while the surrounding tissues (including subcutaneous fat and scar tissue) reflect the light. After the instrument captures this information, it will project the shape of the veins back to the skin surface in real time with dark lines or bright colors.
How to avoid scars: Scar tissue itself lacks normal capillaries and venous networks, so under an imager, the scar area usually appears as a “blank” or blocked zone.
The operator can hold the imaging instrument to scan around the scar and observe the course of the veins (vascular tree).
Search for available veins: Follow the dark vascular lines displayed by the imaging instrument and trace upstream (proximal end) or downstream (distal end) to find a section of vein that avoids the scar edge, has a clear and straight line, and serves as the puncture point.
2-Ultrasonic guidance technology
When the scar area is large or the superficial veins have been exhausted and it is necessary to find deeper veins, ultrasound is the “gold standard”.
Working principle: Utilize high-frequency sound waves to penetrate tissues. Liquids (such as blood in veins) appear black (anechoic) under ultrasound, while dense tissues (such as scars and muscle fascia) appear bright white (hyperechoic).
How to avoid scars
Scar tissue is composed of dense fibrous connective tissue. On an ultrasound screen, it appears as a particularly bright area. Due to its high density, it may produce acoustic shadows at the bottom of the image, blocking the view.
The operator places the ultrasound probe (usually a high-frequency linear array probe) on the normal skin around the scar for cross-sectional scanning.
Search for available veins: Look for black, circular lumens on the ultrasound screen. To confirm that it is a healthy vein rather than an artery or a dead lumen compressed by a scar, the operator will conduct a compression test (gently press down with a probe; a healthy vein is easily flattened and closed, and returns to its original round shape when released). Once the vein is confirmed to be unobstructed, a needle can be inserted through healthy skin without scars under the real-time dynamic guidance of ultrasound.
Key advice: Absolutely avoid inserting or penetrating the needle directly into or through the scar tissue. The pain nerve endings in the scar area may be abnormally sensitive, and due to the lack of normal tissue elasticity, leakage, catheter rupture or phlebitis is very likely to occur after puncture. The greatest value of imaging technology lies in providing you with a "subcutaneous map", allowing you to bypass obstacles and plan the optimal puncture path.
Interested in becoming a distributor? Contact us for wholesale pricing.
Also welcome to contact us, we are ZD Medical Inc.
Tel : +86-187 9586 9515
Email : sales@zd-med.com
Whatsapp/Mobile : +86-187 9586 9515