Integrating Poclight Bench-top CLIA into Decentralized Women’s Endocrine Care Settings
Sex hormone testing is often pigeonholed into fertility, but its impact spans a woman’s entire life.
This International Women’s Day, Poclight celebrates the resilience and intricate biology of women worldwide. We believe that the highest form of care is Precision. We empower every woman with the data she needs to understand her body at every milestone. Our mission is to transform complex clinical questions into clear and immediate answers.
I. Identifying Unmet Needs in Endocrine Care
Hormonal imbalances are often underdiagnosed, leading to long-term health risks that extend far beyond reproductive concerns. Addressing these gaps is the first step toward integrated women's wellness.
● A Case for Early Detection: Polycystic Ovary Syndrome (PCOS) affects up to 13% of women of reproductive age. According to the World Health Organization (WHO), up to 70% of these cases remain undiagnosed globally, often leading to unmanaged metabolic risks.
● The Transition: By 2030, an estimated 1.2 billion women will be navigating the menopausal transition (Source: North American Menopause Society). Without precise monitoring of estrogen decline, risks such as Osteoporosis (which affects 1 in 3 women over the age of 50 according to the International Osteoporosis Foundation) often remain undetected until a fracture occurs.
II. The Clinical Roadmap: When to Test
Regular hormonal profiling is not merely a tool for fertility but a diagnostic necessity to mitigate the long-term risks of metabolic dysfunction, premature aging, and bone density loss.
By identifying physiological shifts early, healthcare providers can implement evidence-based interventions that safeguard a woman’s health long before symptoms become severe.
Clinical Monitoring & Risk Mitigation
Life Stage / Clinical Focus |
Recommended Test Frequency |
Key Biomarkers |
Clinical Objective (Risk Mitigation) |
Adolescence (Pubertal Development) |
Baseline Screening (Annual follow-up) |
FSH, LH, Estradiol (E2) |
To monitor pubertal progression and detect early signs of Precocious Puberty or endocrine metabolic shifts. |
Preventive Wellness (Ages 18–35) |
Every 1 to 2 Years |
AMH, Testosterone, Prolactin (PRL) |
To screen for asymptomatic Polycystic Ovary Syndrome (PCOS) and mitigate risks of long-term metabolic dysfunction. |
Fertility & Family Planning |
Cycle-Specific Tracking |
AMH, Progesterone, LH |
To assess ovarian reserve and confirm ovulation quality, reducing the risk of undiagnosed Infertility. |
Perimenopause (Ages 35–50) |
Every 6 to 12 Months |
FSH, Estradiol (E2), AMH |
To identify Premature Ovarian Insufficiency (POI) and manage the transition to prevent sudden hormonal drops. |
Post-Menopause (Age 50+) |
Annually (Part of geriatric screening) |
FSH, Estradiol (E2) |
To monitor Estrogen deficiency and mitigate the risk of Osteoporosis and cardiovascular complications. |
III. Our Solution: The Poclight C5000 Micro CLIA System
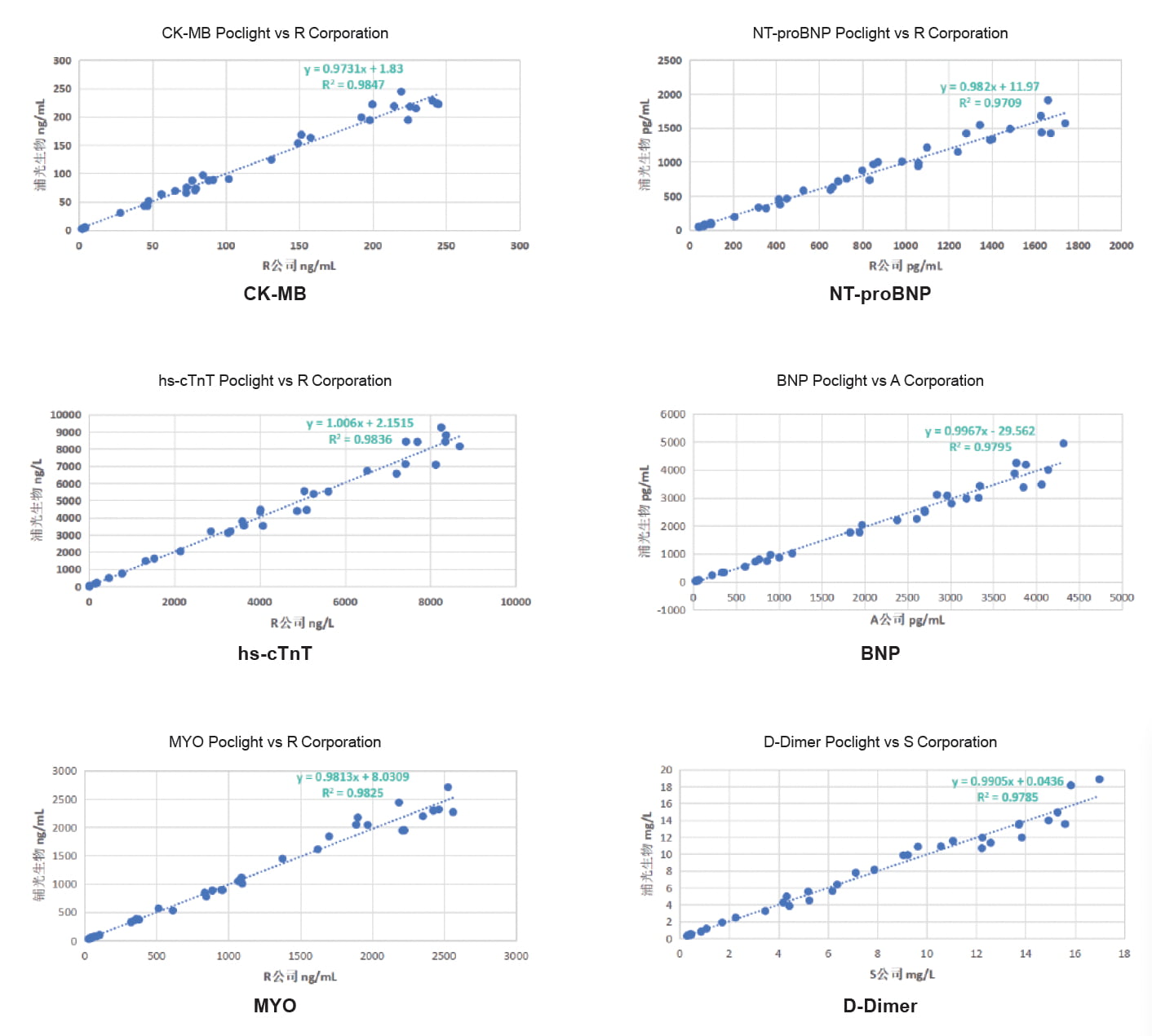
To address these clinical needs at the point of care, the Poclight C5000 Micro CLIA (Chemiluminescence Immunoassay) system provides laboratory-grade precision in a compact format.
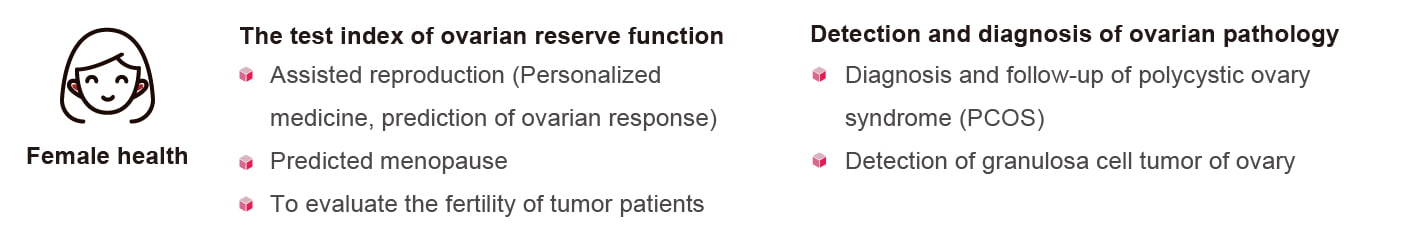
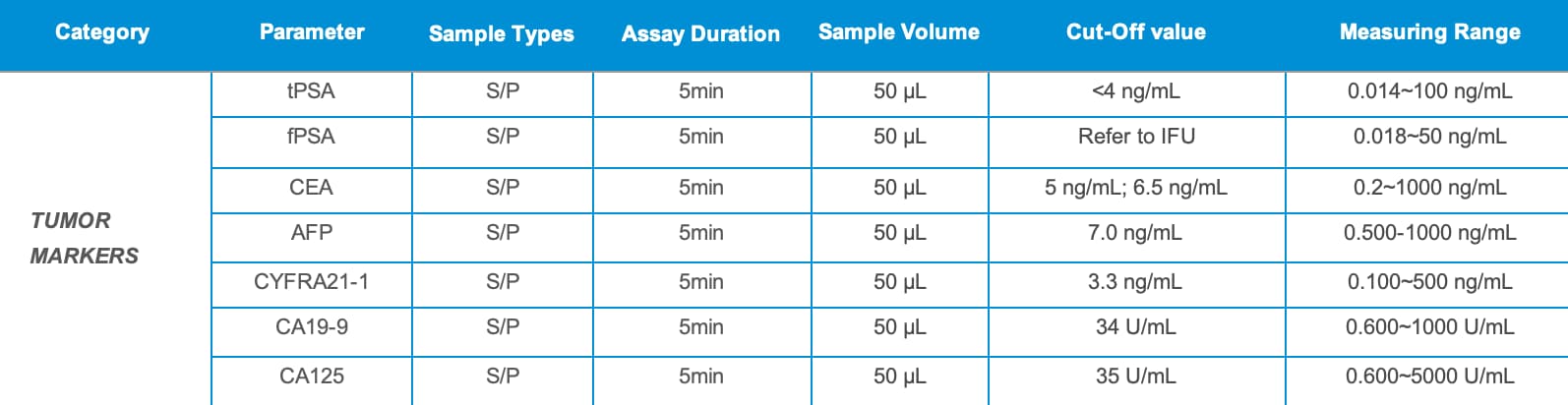
Available hormone fertility markers at a glance:
Discover more about our solutions:
Anti-Müllerian Hormone (AMH) Test Kit
Our standout features:
1. Small Sample Volume & Rapid Results
Only 50 μL of serum or plasma needed, with 5-minute turnaround, ideal for fast clinical decisions.
2. Freeze-dried reagents: no cold chain, 18 months shelf life, simplifying storage and transport.
3. High accuracy and excellent precision (CV < 5%)
4. Applicable with the C5000 POC CLIA Analyzer: 3-Step Operation, Maintenance-Free

Become a Partner / Request a Quote
Are you ready to lead the revolution in decentralized immunology? We invite distributors and healthcare professionals to explore our comprehensive diagnostic panels.