Holding hands and looking at the eyes to help with diagnosis | Suddenly
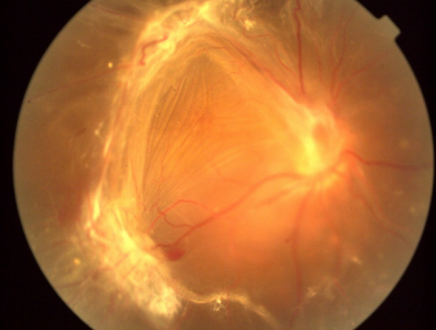
Common causes: tractional retinal detachment (TRD) is mainly caused by the traction of the fibrous vascular membrane on the surface of the retina or within the vitreous. Adult TRD is most commonly seen in proliferative diabetic retinopathy (PDR), retinal vein occlusion (RVO), retinal vasculitis and proliferative vitreoretinopathy (PVR). In addition, trauma, sickle cell retinopathy and uveitis, etc. can also lead to TRD. TRD in children is commonly seen in congenital diseases such as familial exudative vitreoretinopathy (FEVR), retinopathy of prematurity (ROP), and persistent primary vitreous hyperplasia (PHPV).
Clinical manifestations: The patient's symptoms are closely related to the location and extent of the traction. Typical manifestations include: Decreased vision: Posterior pole detachment can cause a sharp decline in central vision, while early peripheral detachment may be asymptomatic. Visual field defect: Fixed direction black shadow occlusion, a certain area of the visual field: "curtain" -like occlusion. Floaters and flashes of light: When the eyes move, brief "lightning-like" or "fire-like" flashes appear before the eyes, mostly around the visual field. Sudden drop in central vision + distorted vision: This highly indicates macular involvement. If not treated promptly, it may cause irreversible vision damage, such as scar formation and photoreceptor cell necrosis.
Diagnostic method: Fundus examination: After mydriasis dilation, the indirect ophthalmoscope can reveal the fibrous vascular membrane and its traction on the retina, with or without vitreous hemorrhage. Optical coherence tomography (OCT) : High-resolution display of the morphology of each layer of the retina, assessment of the position of the traction membrane and the involvement of the macular area. B-ultrasound: It is suitable for patients with severe vitreous opacity to assess the degree of traction and the extent of detachment. Fluorescein fundus angiography: It helps identify neovascularization, non-perfusion areas and lesion distribution, which is beneficial for surgical planning.
Treatment and prognosis: Vitrectomy (PPV) : Removing the proliferative membrane and releasing traction, combined with gas or silicone oil filling to reposition the retina, is the preferred surgical method for TRD. Laser photocoagulation: Targeting ischemic areas or around holes, it reduces new blood vessels and leakage. Anti-vegf drugs: Preoperative injection can reduce the vascular activity of the proliferative membrane and lower the risk of intraoperative bleeding. External scleral compression surgery: It is suitable for peripheral detachment and reduces vitreous traction through external pressure. Postoperative management: Regular follow-up is necessary. Avoid strenuous exercise and intraocular pressure fluctuations. Supplement neurotrophic drugs (such as vitamin B1 and adenosine triphosphate) to promote functional recovery.
Preventive strategies: Control underlying diseases: For instance, patients with diabetes and hypertension need to strictly manage their blood sugar and blood pressure to delay the progression of retinopathy. Regular ophthalmic screening: High-risk groups (patients with high myopia and diabetes) should have fundus examinations every year. Avoid ocular trauma: Especially for those engaged in high-risk occupations, protective equipment should be worn. Timely treatment of vitreous hemorrhage: Early intervention can reduce the formation of organized membranes.
The symptoms of tractional retinal detachment are centered around painless visual abnormalities. In the early stage, they may only present as mild floaters or flashes, which are easily overlooked. As the traction intensifies, visual field defects, distorted vision and decreased vision gradually occur. Due to the significant individual differences in symptoms, especially among high-risk groups such as diabetes and high myopia, even if there are no obvious discomforts, regular fundus screening (such as OCT and fundus fluorescein angiography) is still necessary to avoid delaying treatment due to "asymptomatic" conditions. Once the above warning signals occur, it is essential to visit an ophthalmologist as soon as possible and undergo surgery (such as vitrectomy) to relieve the traction and reposition the retina, so as to save vision to the greatest extent.
Also welcome to contact us, we are ZD Medical Inc.
Tel : +86-187 9586 9515
Email : sales@zd-med.com
Whatsapp/Mobile : +86-187 9586 9515


